Cancer. Even the word carries weight. But if there’s one thing modern medicine is proving, it’s that the narrative around cancer is changing—and fast. Gone are the days when diagnosis automatically meant despair. Today, new therapies, breakthroughs in research, and ultra-personalized treatments are extending lives, shrinking tumors, and sometimes, eliminating cancer entirely.
We’re not talking about hypothetical science fiction here—these advances are already in play, improving patient outcomes in real time. From immune-boosting treatments to genomic targeting and blood tests that catch cancer before it has a name, there are real reasons to be hopeful. Here are 13 advances that are shifting the cancer conversation from fear to fight—and even, in some cases, to freedom.
1. Immunotherapy That Trains Your Body To Fight

Instead of poisoning cancer cells with chemo or burning them away with radiation, immunotherapy helps your immune system recognize and attack tumors on its own. It’s particularly game-changing for hard-to-treat cancers like melanoma and lung cancer. According to Cancer Research Institute, this approach has already helped some patients reach long-term remission where traditional therapies failed.
The best part? Immunotherapy tends to come with fewer debilitating side effects than chemotherapy. It’s like handing your body a more precise weapon—and letting it fight smarter. This isn’t a miracle, but it’s real, and it’s changing lives every single day.
2. CAR T-Cell Therapy
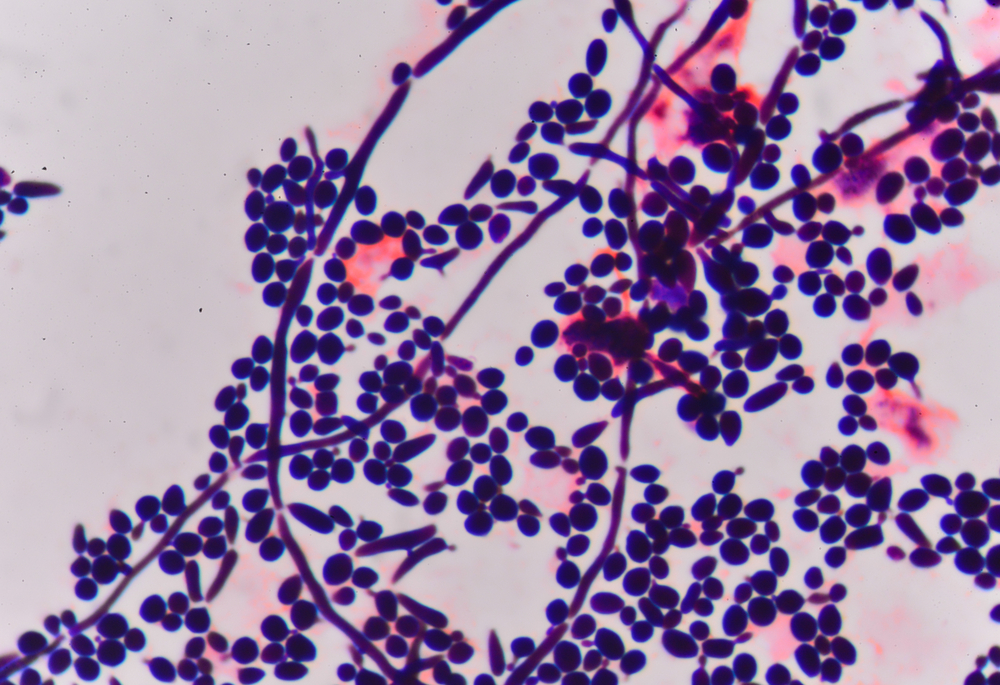
CAR T-cell therapy is one of the most buzzed-about advances in modern oncology—and for good reason. Scientists collect a patient’s T-cells, genetically modify them to better recognize cancer, then reintroduce them into the body like mini assassins. According to Mayo Clinic, it has shown remarkable success in treating blood cancers, especially in patients who had no other options left.
While it’s not without risks and isn’t yet available for all cancer types, it represents a powerful example of personalized medicine. It’s the ultimate plot twist: using your own immune system as a targeted cancer therapy. And it’s not theoretical—it’s saving lives right now.
3. Liquid Biopsies For Early Detection
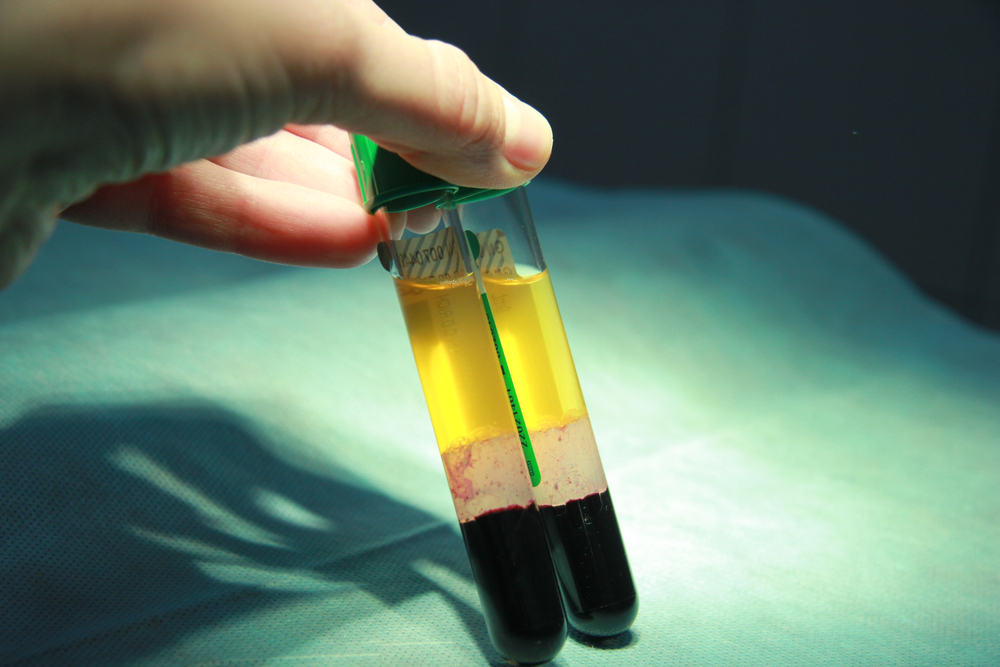
Imagine detecting cancer from a single vial of blood, long before it becomes a visible tumor. That’s the promise of liquid biopsies, which search for circulating tumor DNA (ctDNA) in the bloodstream. According to Johns Hopkins Medicine, these tests are already being used to monitor treatment effectiveness and detect cancer recurrence faster than traditional imaging.
Early detection means earlier intervention, and that changes everything. These tests are also noninvasive, making them more accessible for regular screening. It’s a glimpse into a future where cancer isn’t found late—it’s found early, when it’s most treatable.
4. Precision Medicine Tailored To Your DNA

Precision medicine utilizes your genetic makeup—not just your symptoms—to inform treatment, according to the National Institutes of Health. Instead of a one-size-fits-all approach, doctors can now identify mutations that drive your specific cancer and choose drugs that target those exact changes. It’s already proving effective in breast, lung, and colorectal cancers.
This is where science meets personalization. It gives patients better outcomes with fewer side effects because the therapy is tailored, not generalized. The more we understand your biology, the more precise the treatment becomes.
5. Targeted Therapies That Hit The Bullseye

Unlike chemo, which blasts everything in its path, targeted therapies go after cancer cells like a heat-seeking missile. These drugs latch onto specific proteins or genes that fuel cancer growth, disrupting the disease without decimating your healthy tissue. They’ve become especially effective in breast cancer (HER2-positive), chronic myeloid leukemia, and more.
It’s not about wiping out everything—it’s about precision destruction. And with fewer side effects, many patients can stay stronger, longer, throughout treatment. This is science with surgical finesse.
6. Vaccines That Prevent (And Maybe One Day, Treat) Cancer

HPV vaccines have already dramatically reduced cervical cancer risk, and more cancer-preventing vaccines are in development. But researchers are now exploring therapeutic cancer vaccines—formulas designed not just to prevent, but to treat active cancer by training the immune system to destroy it. It’s a radically different perspective on how we approach disease prevention.
This shift from reactive to proactive medicine could be the game-changer. If successful, cancer vaccines could reduce recurrence and offer new hope for chronic or hard-to-treat cancers. It’s not just about curing—it’s about stopping cancer before it starts.
7. Artificial Intelligence That Predicts Outcomes

AI isn’t just making headlines in tech—it’s revolutionizing oncology. Algorithms can now analyze thousands of patient records, tumor images, and treatment responses to predict what therapies will work best. In some hospitals, AI is already helping pathologists detect cancer earlier and more accurately than the human eye alone.
This doesn’t replace doctors—it empowers them. With better data comes better decision-making, and patients benefit from more effective, tailored care. It’s machine learning, meeting human healing.
8. Radiation That’s Sharper And Safer

Modern radiation therapy is nothing like what it was 20 years ago. Today’s technology enables the ultra-precise targeting of tumors, minimizing damage to surrounding tissues. Techniques like proton beam therapy and stereotactic body radiation therapy (SBRT) are making it possible to treat tumors once considered too risky to zap.
This evolution means fewer side effects, faster recovery, and better tumor control. It’s precision that wasn’t possible a decade ago—and it’s changing treatment outcomes. Radiation doesn’t have to be blunt force anymore.
9. Microbiome-Based Therapies

Your gut health could hold surprising keys to cancer treatment. Research shows that the composition of your microbiome can affect how you respond to immunotherapy. Some trials are even exploring fecal transplants to “reset” the gut and improve immune function during treatment.
It’s weird. It’s wild. And it’s working. The link between gut health and cancer resilience is becoming impossible to ignore—and could shape the next wave of therapy innovation.
10. Epigenetic Drugs That “Reprogram” Cancer

What if you could turn cancer genes off like a light switch? That’s the promise of epigenetic drugs—treatments that change how genes behave without altering the underlying DNA. These drugs are being explored in blood cancers and some solid tumors with promising early results.
By reprogramming cancer cells to behave more like normal cells—or making them more sensitive to existing therapies—these drugs add a whole new layer to the oncology toolkit. They’re not a silver bullet, but they’re a powerful addition to the arsenal.
11. Clinical Trials That Are Easier To Join
Access to groundbreaking treatments used to be limited to those living near major hospitals. Now, decentralized clinical trials and digital platforms are making participation easier than ever. Patients can enroll online, use wearable monitors, and even have medications shipped to their homes.
This democratizes access to innovation. It means more people get cutting-edge care—now, not five years from now. And the more diverse and robust the trials, the faster progress accelerates.
12. Integrative Care That Treats The Whole Person

Modern cancer treatment is finally embracing holistic care, not as an afterthought, but as part of the plan. That includes nutrition, mental health, acupuncture, exercise, and even mindfulness. These aren’t woo-woo extras—they improve outcomes, quality of life, and recovery.
Patients who feel better do better. And many hospitals now include integrative medicine as a formal part of cancer care. It’s science with soul.
13. Survivorship Plans That Look Beyond “Cure”

Cancer treatment doesn’t end when the chemo stops. Survivorship care plans are helping patients transition from treatment to long-term health, with support for emotional well-being, hormonal balance, and recurrence prevention. This holistic follow-up care is becoming standard—and it’s saving lives.
Because surviving cancer is just one chapter. Thriving after it? That’s the goal now. And modern oncology is finally making space for that narrative.

Abisola is a communication specialist with a background in language studies and project management. She believes in the power of words to effectively connect with her audience and address their needs. With her strong foundation in both language and project management, she crafts messages that are not only clear and engaging but also aligned with strategic goals. Whether through content creation, storytelling, or communication planning, Abisola uses her expertise to ensure that her messages resonate and deliver lasting value to her audience.


